Ocular proptosis is the protrusion of the eye from its socket.
Brachycephalic breeds of dog, such as shih tzu’s, pugs, bulldogs, and pekingese dogs are well-represented in cases of ocular proptosis. This is due to their facial structure wherein their eye sockets are shallow, making it easy for the dog’s eyes to bulge out.


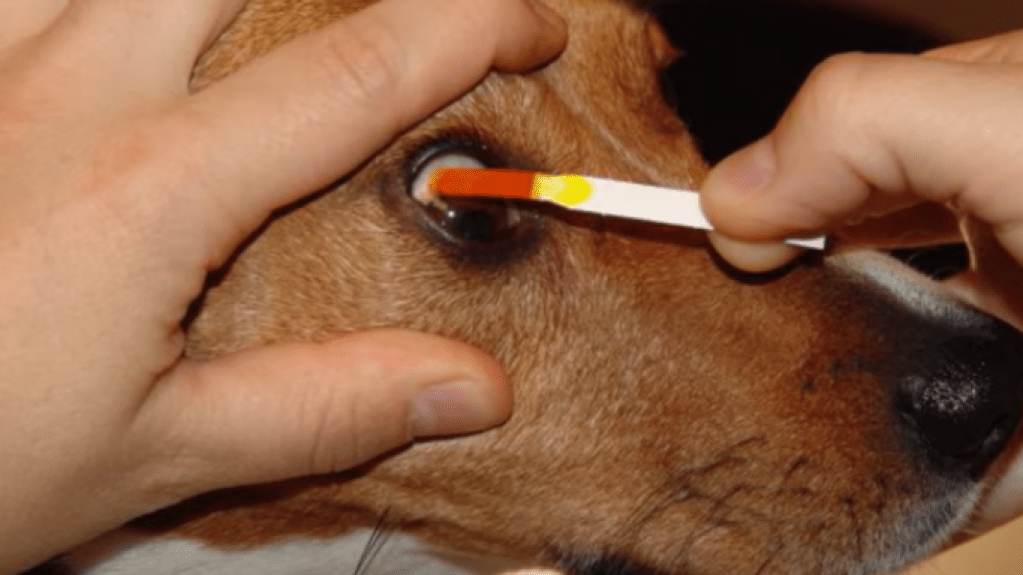
Right: Healthy eye after treatment.
Ocular proptosis should be treated as an emergency. The mere dryness of the overexposed eye (corneal desiccation) can lead to corneal ulceration. There is also high risk of blindness, among other complications.
Table of Contents
- Symptoms of Ocular Proptosis
- First Aid for Ocular Proptosis
- Causes of Ocular Proptosis
- Treatment Methods for Ocular Proptosis
- Ocular Proptosis Case
- Ocular Proptosis FAQs
Symptoms
Proptosis is relatively easy to detect through physical inspection. The affected eye may be completely protruding or only slightly.
If a pet owner is unsure if the eye is indeed bulging, here are things to look out for:
- Uneven eyes (affected eye is protruding)
- Strabismus (cross-eye)
- Corneal desiccation (dry eye) when at least 1 hour has elapsed
- Conjunctivitis, reddish blood vessels in eye

It also helps to view the dog’s eye from the side or from the top of their head, as this may make the difference in the size of the two eyes more apparent than if they are viewed upfront.
Causes
The main cause of proptosis is trauma such as those from falls and dog fights.
This may not only be trauma near the eyes, but also on certain parts of the body such as the neck.
When it comes to brachycephalic breeds with protruding eyes such as pugs and bulldogs, even pressure on the neck from a collar may result in ocular proptosis due to their facial structure having shallow eye sockets.
Although not as common as trauma, pressure from tumors at the back of the eye may also lead to it bulging out.
First Aid
Ocular proptosis requires immediate attention. If your dog or small animal’s eye protrudes from its socket, follow these steps:
- Find a clean piece of cloth.
- Dampen it.
- Gently cover the animal’s eye.
- Call your vet and bring the animal to the clinic.
If the dog hasn’t eaten yet, that’s fine. Give them water, or if they’re overdue for feeding, limit the amount of food you give; although the procedure will be on their eye, it’s likely that they’ll need their stomach empty in preparation for surgery.
Treatment Methods
Treatment depends on the severity of the proptosis, as well as the pet owner’s capacity for long-term care.

Eyeball Replacement
Eyeball replacement, or globe replacement, involves helping the eyeball re-align with the eye socket through temporary tarsorrhaphy.
Tarsorrhaphy is a surgical procedure wherein the eyelids are sewn together. In temporary tarsorrhaphy, this is done to protect the eye and facilitate recovery until the eye is healed enough to be un-sewn.
Eyeball replacement is generally more preferred over irreversible enucleation.
Eyeball replacement is apt for patient dogs who have mild cases of ocular proptosis and whose eyeball can be salvaged and is aesthetically satisfactory to the pet owner.
Enucleation
Enucleation or complete removal of the dog’s eye is considered when all other options have been exhausted.
If the patient is a strong candidate for enucleation, enucleation may also be the chosen procedure, without having the animal first undergo eyeball replacement.
A patient with proptosis is a strong candidate for enucleation if the optic nerves of the affected eye are broken, or if there is hemorrhage, infection, tumor, or advanced glaucoma.
For pet owners unable or hesitant to provide long-term care, enucleation is also considered.
Recovery
After surgery, the patient recovering from ocular proptosis may experience strabismus or cross eye. This may last 3 to 6 months, sometimes 9 depending on different factors, after which the eye may return to normal.
Said factors affecting prognosis are:
- duration of corneal exposure
- breed
- damage to the eye and its surroundings
Case
Ocular Proptosis FAQs
What breeds are prone to ocular proptosis?
Breeds with protruding eyes are prone to proptosis. These include pugs, bulldogs, shih-tzu’s, and Pekingese.
Does my pug have proptosis? I can’t tell because his eyes are always bulging.
A simple way to check is to compare one eye to the other. It also helps to observe the eye from the side or from the top of the dog’s head, rather than from the front. See also: symptoms.
My dog’s breed is prone to ocular proptosis. How do I prevent him from getting it?
Review the causes. Here is a non-exhaustive list of preventive measures:
- Neuter your pet. In prone breeds, proptosis may result from tugs at the collar or leash, such as when preventing them from entering into a dog fight.
- Socialize your pet with other dogs. As with neutering, the goal here is to make your dog less prone to aggression, so there will be no need to pull them from the collar and less sources of trauma.
- Beware of other dogs. If you can, pick up your dog and keep them away from unfamiliar dogs that may initiate the dog fight.
Will my dog become blind from proptosis?
It depends on the severity of the case.
My dog’s eye is protruding. Can it go back in?
A vet may professionally restore the eye. However, this depends on the its state.
See also: Will my dog lose his eye?
Will my dog lose his eye from traumatic proptosis?
It depends on the state of his eye.
Damaged optic nerves, hemorrhage, infection, tumor, and advanced glaucoma are some of the considerations that go into deciding whether enucleation is an appropriate treatment method.
If the eye is in a good state, it may simply be replaced. See Treatment Methods.